Basic Principles
Assessing Severity of Pain
Pain assessment is essential to identify whether a patient has pain, how severe it is, and whether the intervention to treat it has been successful.
The patient should be asked to rate both their
- pain at rest to guide prescribing for background pain (constant), and
- pain on movement (coughing, being rolled, walking with the physio) to guide prescribing for breakthrough pain (intermittent).
There are numerous pain assessment tools.
- VRS - verbal rating scale VRS - Verbal Rating Scale - MOST COMMONLY USED
- NRS - numerical rating scale NRS - Numerical Rating Scale
- VAS - visual analogue scale VAS - Visual Analogue Scale
- Wong-Baker faces scale For Children - Wong Baker Faces Scale
- r-FLACC scale For Children or non-verbal Adults - FLACC
- Abbey Pain Scale For Patients with Dementia - Abbey Pain Scale
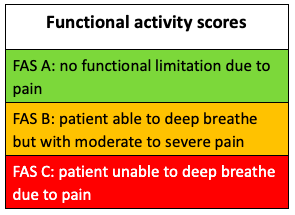
We also now use the Functional Activity Score to assess the impact of pain on function. The function measured is related to the surgery or injury: we may want to assess a patient's ability to comply with physiotherapy after a knee replacement, or the ability to take a deep breath and cough in a patient with rib fractures, as in the example below.