Basic Management of Pain
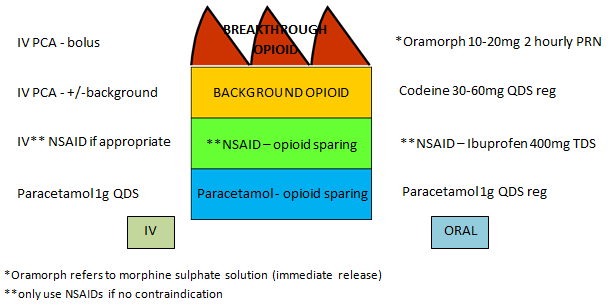
The diagram below shows how basic analgesia should be built up to provide good pain control in most situations, with regular analgesia prescribed for background pain and prn analgesia prescribed for intermittent, breakthrough pain. The left side shows intravenous (IV) administration and the right side oral administration. IV should only be used if the patient is unable to absorb analgesia orally ( Starting a PCA ).
Prescribing a range of doses for the opioids allows the patient to find the right dose for them.
If pain is not initially felt to be severe the analgesic plan can be started with PRN weak opioids (eg Codeine), and then increased if pain is not well controlled. Similarly, as tissue injury resolves and acute pain diminishes, the analgesic plan can be stepped down accordingly:
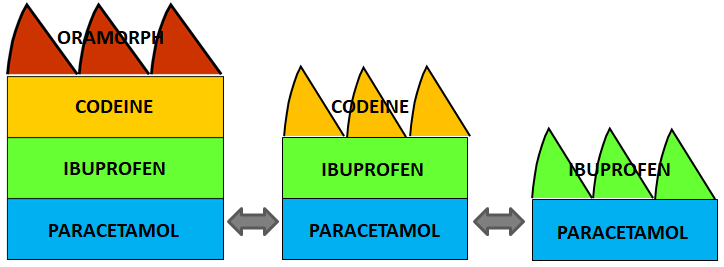
Conversely, if pain is severe despite regular opioid-sparing and weak opioid analgesia, and pro-active use of PRN strong opioids, then the weak opioid could be replaced by regular QDS strong opioids (eg Morphine immediate release), and the PRN Morphine continued.
Please note: modified release opioid preparations should not be initiated for patients with acute pain - Prolonged-release opioids: Removal of indication for relief of post-operative pain - GOV.UK
Drugs used for the management of acute pain:
Paracetamol Ibuprofen Naproxen Diclofenac Codeine Tramadol Dihydrocodeine Morphine Oxycodone
Remember that pain itself causes nausea and opioid analgesia will make this worse – always co-prescribe an antiemetic, and a laxative to prevent constipation.
Management of nausea and vomiting in adults-OUH MIL
Management of acute constipation in adults-OUH MIL
