Anaesthetists Only
Out of Hours Acute Pain Management for Anaesthetists
The following guidance is designed as a support tool for anaesthetists only, to guide pain management for:
- adult patients over the age of 18
- weight more than 50kg
- paediatric algorithms should be used for younger and lighter patients
- normal renal and hepatic function
- drug doses should be reduced, or the drug may be contraindicated, in patients with co-morbidities.
This guidance does not take into account the individual circumstances of the patient and may not contain all the information required. It must not be used as the sole basis for prescribing any drugs or for the care of any patient.
Basic Management of Pain
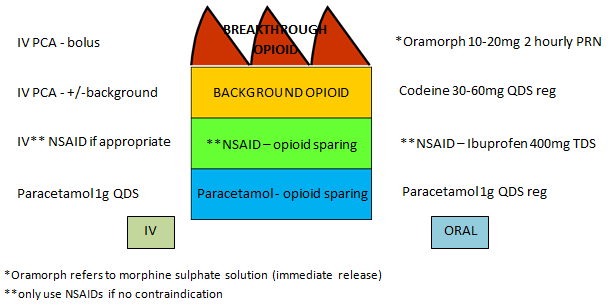
Most patients do well with regular analgesia (opioid-sparing agents such as paracetamol and NSAID together with a weak opioid) prescribed for background pain and prn strong opioid analgesia prescribed for intermittent, breakthrough pain, such as during physiotherapy, mobilising or dressing changes. The left shows intravenous (IV) administration and the right oral administration.
Multimodal Analgesia for Nociceptive (Acute) Pain
Optimise Local Anaesthetic Infusions
- ensure catheter is correctly positioned and hasn't migrated
- increase infusion rate or consider bolus (only to be given by anaesthetist)
- resite if necessary this is particularly important BEFORE a patient leaves a critical care or high dependency area
- it should also be strongly considered during daylight hours if the epidural had been problematic during the previous night
Optimise PCA
Please follow link to Pain Despite PCA
Non- Pharmacological Management of Pain
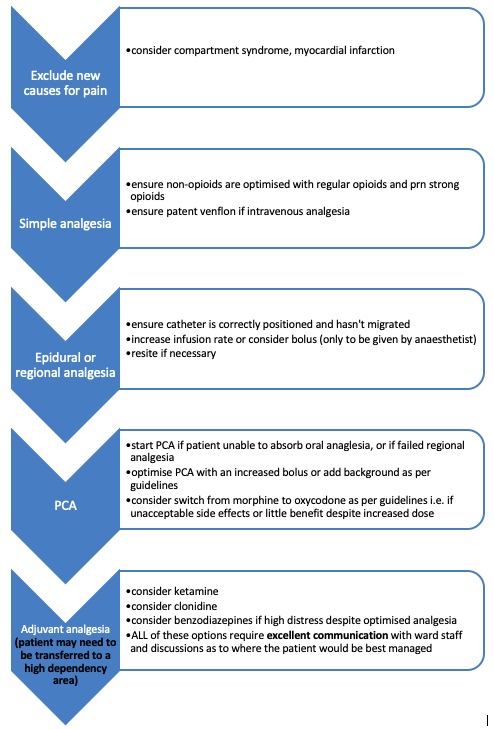
If a patient is in severe pain, first exclude complications such as compartment syndrome, ischaemia, bowel perforation, cardiac event.
It is important to remember that pain is exacerbated by anxiety, distress and depression, so a holistic approach is important. In anxiety, excitatory descending pathways from the brain to the spinal cord will increase the sensitivity of the pain system.
Conversely, inhibitory descending pathways can be engaged with relaxation, distraction and reassurance, thus decreasing the experience of pain.
Other non-pharmacological methods of pain management include splinting fractures, dressing wounds, changing mattresses or chairs for more comfort, elevation of the limb, physiotherapy to address muscle spasm, heat or ice packs.
If the pain and distress experienced appear greater than that expected, acute pathology has been ruled out, and sufficient multimodal analgesia provided, it is important to ask the patient what they think is the cause of their pain. Occasionally patients may have mistaken ideas about their pain which in itself increases anxiety and distress, leading to increased pain. This may include an assumption that pain indicates a recurrence of cancer, a complication of surgery or a diagnosis that is being hidden from them. As well as ensuring that adequate analgesia is available, these patients benefit from clear, careful explanations and reassurance.
Adjuvant Analgesia- Ketamine
*Many wards will not be happy to nurse patients with a low-dose ketamine infusion, so communicate well with the ward staff, and consider transferring the patient to a higher dependence area if necessary.*
Ketamine should be used with caution as many patients find the hallucinations or dreams disturbing. Patients should be warned of these effects and told to inform staff if they experience anything distressing so that the infusion can be stopped. Staff may also decide to stop the infusion if the patient looks afraid or acts oddly, as ketamine can occasionally produce a “locked in” effect. Nursing the patient in a quiet environment helps.
Indications: Adult patients where multimodal analgesia – paracetamol, NSAIDs, opioids, +/- local anaesthetic block – has failed to produce satisfactory analgesia, despite appropriate opioid dose escalation and optimisation of the opioid PCA. Most patients will not require ketamine, but it can prove useful in complex pain.
Ensure that the patient understands the risk of dysphoria as some patients will choose not to consent.
Contraindications:
- Raised intracranial pressure or intracranial space occupying lesion.
- Cardiac arrhythmia or severe systemic hypertension.
- Raised intra-ocular pressure.
- Recent history of epilepsy.
- Recent history of psychosis.
Ketamine should be used with caution in patients on long-acting opioids, as it can increase opioid sensitivity and risk respiratory depression and sedation.
Side effects: Dysphoria, hallucinations, drowsiness, vivid dreams, dizziness, palpitations, hypertension, nausea and features of opioid toxicity.
Dose: Initial slow iv bolus dose of 0.1 - 0.5mg/kg, so 7mg - 35mg in a 70kg man (using ideal body weight IBW*). Give the dose incrementally and wait between increments to ensure the patient is not experiencing dysphoria. If no benefit from the bolus dose, an infusion should not be started.
Usual ketamine iv or sc infusion dose is 0.1mg/kg/hr, so 7mg/hr in a 70kg man (IBW). The prescription for this can be found on ePMA under Acute Pain Powerplan.
[Higher doses of ketamine do not give an increased morphine-sparing effect but will increase the risk of psychotomimetic effects].
Preparation: Dilute one vial of 20ml (=200mg) ketamine up to 40ml with 0.9% saline, to give a concentration of 5mg/ml. [Check the vial concentration as there are different strengths of solution].
Oral doses: start at 0.5mg/kg tds, and then increase the doses by 0.5mg/kg as tolerated.
Clonidine
*Many wards will not be happy to nurse patients with a low-dose clonidine infusion, so communicate well with the ward staff, and consider transferring the patient to a higher dependence area if necessary.*
Clonidine should be used with caution due to hypotension and sedation.
Indications: Adult patients where mulitmodal analgesia - paracetamol, NSAIDs, opioids +/- local anaesthetic block - has failed to produce satisfactory analgesia, despite appropriate opioid escalation and optimisation of the opioid PCA. Most patients will not require clonidine, but it can prove useful in patients with complex pain.
Clonidine should be used with caution in patients on concurrent opioidds or benzodiazepines, as it can increase opioid sensitivity and risk respiratory depression and sedation.
Side effects: Sedation, hypotension.
Dose: Dilute 150mcg clonidine (1ml) with 9ml 0.9% saline to give a 10ml syringe of 15mcg/ml. Titrate boluses of 1-2ml (15-30mcg) and wait 3 minutes before repeating the dose. Do not give if the systolic BP is less than 90, or if the patient becomes sedated. If no benefit from the bolus dose, an infusion should not be started.
Usual clonidine iv or sc infusion dose is 0.3mcg/kg/hr. The prescription for this can be found on ePMA under Acute Pain Powerplan.
Oral doses: start at 25mcg tds, and then increase the doses as tolerated.
Independent of the route of administration, do not give clonidine if the systolic BP is less than 90, or if the clonidine has produced a drop in BP of more than 20% in baseline BP.
Gabapentin/Pregabalin
There is little evidence of the benefits of gabapentinoids in acute post-operative pain. The side effects of sedation, dizziness and visual disturbance preclude their routine use, but they may be of benefit in patients with acute neuropathic pain or those with opioid addiction (although these drugs also have misuse potential).
There are no parenteral formulations for these drugs so the patients must have good enteral absorption. Suggested initial doses in the acute post-operative period:
- Gabapentin 300mg tds
- Pregabalin 25mg bd
- the additional anxiolytic effect of pregabalin may prove beneficial for those patients with pain and high distress
Patients with Opioid Dependence
Please follow link to Analgesia in Patients with Opioid Dependence
Basic principles must acknowledge that these patients are at risk of:
- Opioid induced hyperalgesia
- Increased pain sensitivity
- Need for optimal multimodal analgesia
- Opioid tolerance
- Reduced opioid effectiveness
- Higher opioid dose where needed
- (although side effects are variable so need careful monitoring)
- Gabapentin, pregabalin may be useful in some cases
- Risk of opioid withdrawal if unable to take usual drugs
- Continue baseline opioids
- Monitor with the COWS score (clinical opioid withdrawal scale) – see app
- Clonidine, gabapentin, pregabalin may all mitigate withdrawal symptoms
Patients with Blunt Chest Trauma
Please follow links to the Flowchart for analgesia in blunt chest trauma, which includes a Battle score calculator and a flowsheet for analgesia.
Many of these patients will require a local anaesthetic block for optimum analgesia.
