Elderly Patients
Pain Assessment
Pain is often unrecognised and undertreated in older patients. They may have a pre-existing painful condition such as arthritis as well as pain from their admission diagnosis. Older patients often use different language to describe their pain - “it’s sore, it’s uncomfortable, it aches” – so if a patient denies pain using the usual verbal descriptor scale VRS - Verbal Rating Scale it is important to ask more questions to confirm no discomfort. Patients with severe dementia who are unable to answer direct questions should have pain assessment using the Abbey Pain Scale For Patients with Dementia - Abbey Pain Scale. Carers should be included in the assessment process as they may identify subtle changes in behaviour which may reflect pain.
Pain Management
Studies have shown that ward staff tend to underestimate pain needs, under-prescribe analgesia and under-medicate. This is often related to concerns over co-morbidities or polypharmacy.
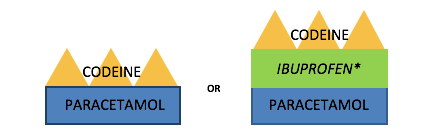
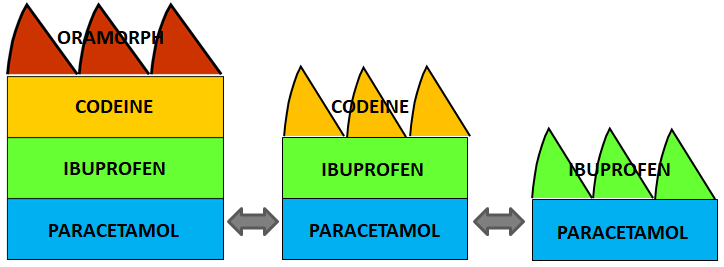
Use a pain ladder approach to analgesia using the safest drugs administered via the safest route first, then escalating treatment if analgesia is ineffective (see Basic Management of Pain) For many analgesics a lower initial dose may be required compared to younger adults, with subsequent doses titrated to response.
Analgesia is important to allow mobility and physiotherapy. This will strengthen muscle support of painful joints which will ultimately improve symptoms.
Consider non-pharmacological management of pain (Non Pharmacological Management of Pain ): reassurance, change of bed or chair, splinting of fractures, ulcer dressings.
Contact the pain team if needed for more support and advice. (Useful Contact Details within OUH)
Practical Guidance
- Give regular Paracetamol (for background pain and for the opioid sparing effect)
- Caution with NSAIDs due to higher risk of adverse effects. Avoid if older than 75 years old or 65 if they have renal or cardiac disease.
If younger than 75 years old and no contraindications:
- Use the smallest possible dose for the shortest time necessary*
- Give gastric protection (H2 antagonists are preferred in older patients as proton pump inhibitors increase the risk of Clostridium difficile)
- Initially give prn Codeine 30mg 4hourly (for breakthrough pain)
- Use may be limited by constipation, nausea and confusion
*only use NSAIDs if no contraindication, and use with caution.
If pain is not well controlled, consider increasing background analgesia by giving regular Codeine and adding immediate release Morphine prn at a dose of 5-10mg 2hourly (or starting at 2.5mg if very frail). Morphine doses can be increased as tolerated.
- Tramadol causes fewer respiratory and gastrointestinal side effects than other opioids but is associated with delirium, and can often cause nausea, vomiting, sweating, dizziness, tremors and headaches. It is a weak opioid and is no stronger than codeine. Codeine is generally preferred for the older patient.
- Strong opioids: start low and go slow. Give short-acting opioids (eg Morphine or Oxycodone) 15-30 minutes before an expected painful event such as physiotherapy, mobilisation or rolling in bed.
- Give regular laxatives if opioids are prescribed.
-
Management of constipation MIL: http://ouh.oxnet.nhs.uk/Pharmacy/Mils/MILV8N10.pdf
- Prescribe prn Naloxone (40microgram boluses) if strong opioids are prescribed.
- Consider Gabapentin or Amitriptyline (with caution, see below) for neuropathic pain.
- Depression may be expressed as pain, so a holistic approach is important.
Confusion
Opioids are not the only cause of confusion, so ensure that other causes are sought and excluded, eg hypovolaemia, hypoxia, sepsis (including UTI), electrolyte disturbances, hypo- or hyperglycaemia, renal or hepatic dysfunction, CVA. Confusion is common after a general anaesthetic or after a stay in intensive care.
Pain is also a cause of confusion so stopping analgesia may worsen, not improve, the situation.
If other causes have been excluded and opioids may be contributing to confusion, consider reducing the opioid load by stopping the regular opioids. Ensure that prn opioids are still available for breakthrough pain from mobilisation etc. Consider changing the Morphine to Oxycodone, and record in the notes why oxycodone has been prescribed.
Prescribing strong opioids MIL: http://ouh.oxnet.nhs.uk/Pharmacy/Mils/MILV7N5.pdf
Falls
Polypharmacy in the elderly has been found to increase the risk of falls. Although analgesics themselves do not appear to increase risk, benzodiazepines and tricyclic antidepressants (eg Amitriptyline ) are associated with a high risk of falling so should be used with care.
Medications that contribute to the risk of falls MIL: http://ouh.oxnet.nhs.uk/Pharmacy/Mils/MILV7N6.PDF
